Article Content Antibiotic resistance (AR) has steadily accelerated in recent years to become a global health crisis. As deadly bacteria evolve new ways to elude drug treatments for a variety of illnesses, a growing number of “superbugs” have emerged, ramping up estimates of more than 10 million worldwide deaths per year by 2050. Scientists are
Article Content
Antibiotic resistance (AR) has steadily accelerated in recent years to become a global health crisis. As deadly bacteria evolve new ways to elude drug treatments for a variety of illnesses, a growing number of “superbugs” have emerged, ramping up estimates of more than 10 million worldwide deaths per year by 2050.
Scientists are looking to recently developed technologies to address the pressing threat of antibiotic-resistant bacteria, which are known to flourish in hospital settings, sewage treatment areas, animal husbandry locations and fish farms. University of California San Diego scientists have now applied cutting-edge genetics tools to counteract antibiotic resistance.
The laboratories of UC San Diego School of Biological Sciences Professors Ethan Bier and Justin Meyer have collaborated on a novel method of removing antibiotic-resistant elements from populations of bacteria. The researchers developed a new CRISPR-based technology similar to gene drives, which are being applied in insect populations to disrupt the spread of harmful properties, such as parasites that cause malaria. The new Pro-Active Genetics (Pro-AG) tool called pPro-MobV is a second-generation technology that uses a similar approach to disable drug resistance in populations of bacteria.
“With pPro-MobV we have brought gene-drive thinking from insects to bacteria as a population engineering tool,” said Bier, a faculty member in the Department of Cell and Developmental Biology. “With this new CRISPR-based technology we can take a few cells and let them go to neutralize AR in a large target population.”
In 2019 Bier’s lab collaborated with Professor Victor Nizet’s group (UC San Diego School of Medicine) to develop the initial Pro-AG concept, in which a genetic cassette is introduced and copied between the genomes of bacteria to inactivate their antibiotic-resistant components. The cassette launches itself into an AR gene carried on plasmids, circular types of DNA that replicate within cells, thereby restoring sensitivity of the bacteria to antibiotic treatments.
Building upon this idea, Bier and his colleagues developed a follow-on system that spreads the antibiotic CRISPR cassette components via conjugal transfer, which is similar to mating in bacteria. As they described in the Nature journal npj Antimicrobials and Resistance, the researchers showed that this next-generation pPro-MobV system can exploit a naturally created bacterial mating tunnel between cells to spread the key disabling elements. They demonstrated the process working within bacterial biofilms, which are communities of microorganisms that contaminate various surfaces and can be extremely difficult to remove under conventional cleaning methods. Biofilms also contribute to the spread of disease and are created in the majority of infections that lead to serious disease, in part because biofilms help combat antibiotics by creating a protective layer of cells that is difficult for antibiotics to diffuse through. The new technology therefore carries potential in health care settings, environmental remediation and microbiome engineering.
 Internet Connectz
Internet Connectz 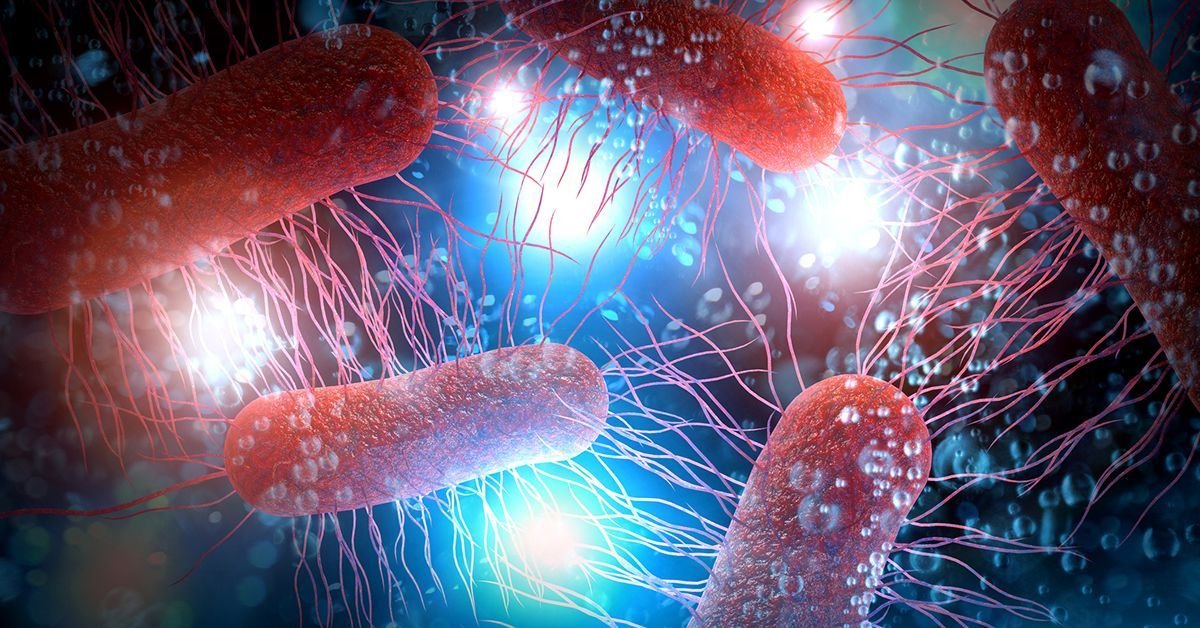












Leave a Comment
Your email address will not be published. Required fields are marked with *